The bone marrow microenvironment plays a pivotal role in the recurrence of acute myeloid leukemia (AML). However, the exact mechanisms are not fully understood. Single-cell technologies have emerged as powerful tools for unraveling the immune microenvironment in leukemia. In this study, utilizing scRNA-seq on a cohort of 13 paired AML patients, we have unveiled a distinctive subcluster of tumor-associated macrophages (TAMs) linked to relapse leukemia.
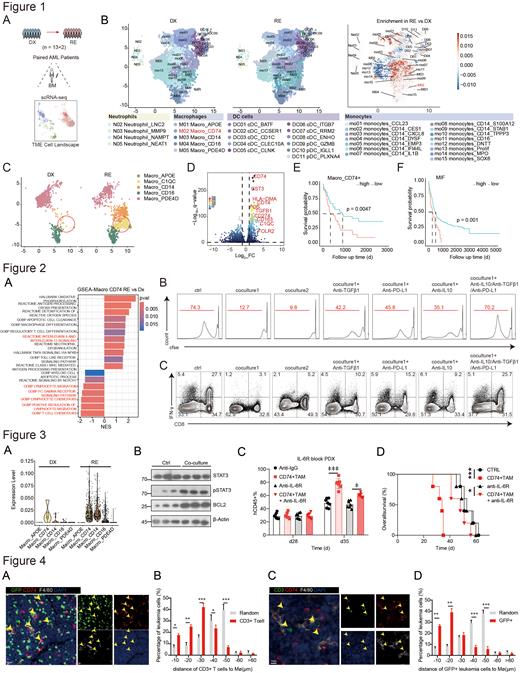
To explore the heterogeneity of the bone marrow microenvironment during the progression of AML, we conducted a scRNA-seq analysis on bone marrow cells obtained from 13 paired AML patients at the time of diagnosis (DX) and relapse (RE) (Figure 1A). Employing UMAP for dimensionality reduction, we detected multiple subclusters and observed a notable rise in the Macrophage CD74 cluster in all paired RE patients, suggesting a pivotal role of CD74+ TAMs in AML relapse (Figure 1B-C). Furthermore, CD274, FOS, TGFβ1, and CD163, recognized as markers of M2 macrophages, were significantly enriched in the CD74+ TAMs population (Figure 1D). Intriguingly, a higher proportion of CD74+ TAMs correlated with unfavorable outcomes in TCGA database (Figure 1E). Meanwhile, we found that the ligand macrophage migration inhibitory factor (MIF) of CD74 was associated with poor prognosis of AML (Figure 1F).
To investigate the association of CD74+ TAMs with AML cells, Gene Set Variation Analysis (GSVA) was employed and revealed restrained pathways related to T cell function (Figure 2A). Through in vitro experiments on patient samples, we found that CD74+TAM can inhibit the proliferation of T cells and the secretion of IFN-γ. Further monoclonal antibody block experiments unveiled that this inhibitory effect might be attributed to the heightened expression of PD-L1, TGFβ1, and IL-10 by the macrophages (Figure 2B-C). In conclusion, we have substantiated the inhibitory role of CD74+ TAMs on T cells, which hampers their ability to engage in effective tumor killing.
To elucidate the interplay between CD74+ TAMs and AML cells, we examined the gene expression profile of cytokines, noting a significant increase in the expression level of IL-6 within the CD74+ TAMs subclusters of the RE group (Figure 3A). Furthermore, upon co-culture with CD74+ TAMs, THP-1 cells exhibited notable activation of IL-6 related pathways (Figure 3B). The injection of CD74+ TAMs resulted in heightened AML initiation and poorer survival in patient-derived xenograft (PDX) model, which was reversed by blocking the IL-6-IL-6R axis (Figure 3C-D). These findings collectively confirm that IL-6 secreted by CD74+ TAMs fosters the malignancy and drug resistance of AML cells.
Subsequently, MLL-AF9-induced AML mouse model was employed to explore the spatial interplay between CD74+ TAMs, AML cells and T cells. Immunofluorescence (IF) analysis of mouse bone marrow tissue revealed that after chemotherapy, the proximity between AML cells and CD74+ TAMs decreased (Figure 4A-B). Conversely, the presence of T cells surrounding CD74+ TAMs increased (Figure 4C-D). These findings indicate that CD74+ TAMs can inhibit T cell function and directly influence AML cells within the tumor microenvironment.
In summary, our study revealed a notable rise in the proportion of TAMs expressing CD74 in relapsed AML patients. These CD74+ TAMs were found to facilitate leukemia progression while concurrently inhibiting T cell immune surveillance in the context of AML. Thus, our findings indicate that CD74+ TAMs represent a distinct type of macrophages associated with AML relapse.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal